Abstract
Objective: Posttransplant infection is common and tough to deal, patients after HSCT rely on immune reconstitution for protection. We desperately need a deeper understanding of how the system works to help the patients overcome the infection.
Method: This study analyzed the disease course of EBV viremia after haplo-HSCT, as well as the laboratory testing data. The sex bias during immune reconstitution was manifested by comparing the outcomes between male and female patients,
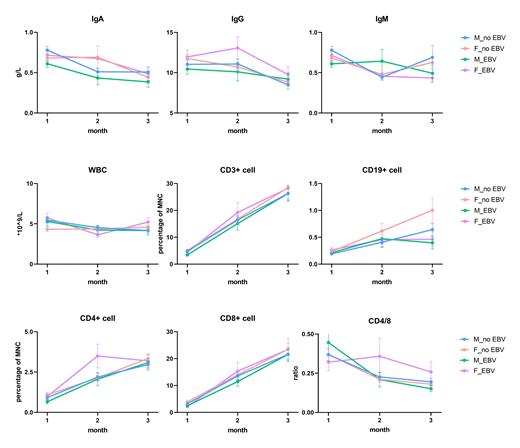
Results: 236 patients received haplo-HSCT in 2013 in our center, at a median follow up of 5 years, among whom 78 patients underwent EBV infection. The incidence of EBV viremia after transplantation is 33.1% in total, with a significant difference between men and women (40.0% and 26.7% respectively, p=0.034). Men tended to have earlier onset time (14-434d after HSCT) and longer duration (7-70d) than women (17-592d after HSCT, 7-30d). Both the initial and peak viral load were higher in men than in women (initial viral load>10 4/ml: men 6.52% vs. women 3.13%, peak viral load>10 5/ml: men 8.70% vs. women 3.13%). To explain this phenomenon, we analyzed the laboratory testing data on 30d and 60d after HSCT. And we found that male patients had higher plasma levels of immunoglobulin M on 60d after HSCT if infected by EBV, referring to more robust induction of innate immune (p=0.033). By contrast, female patients had significantly increased CD4+ T cell during EBV infection, representing more robust activation of adaptive immune (p=0.019).
Conclusion: These findings provide a possible explanation for the observed sex biases in EBV viremia after haplo-HSCT, and provide an important basis for the recognition of immune reconstitution, furthermore, raise concern of the development of a sex-based approach to the treatment and care of male and female patients with infection after HSCT.
No relevant conflicts of interest to declare.